Neurological Disabilites
Cerebral Palsy
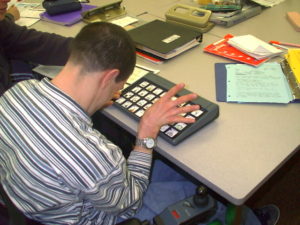
Cerebral palsy is a condition caused by damage to the brain, usually occurring before, during or shortly following birth. “Cerebral” refers to the brain and “palsy” to a disorder of movement or posture. It is neither progressive nor communicable. It is also not “curable” in the accepted sense, although education, therapy, and applied technology can help persons with cerebral palsy lead productive lives. It is not a disease and should never be referred to as such. It can range from mild to severe.
The causes of cerebral palsy include illness during pregnancy, premature delivery, or lack of oxygen supply to the baby; or it may occur early in life as a result of an accident, lead poisoning, viral infection, child abuse, or other factors. Chief among the causes is an insufficient amount of oxygen or poor flow of blood reaching the fetal or newborn brain. Lack of good prenatal care may also be a factor. A less common type is acquired cerebral palsy: head injury is the most frequent cause, usually the result of motor vehicle accidents, falls, or child abuse.
Cerebral palsy is characterized by an inability to fully control motor function. Depending on which part of the brain has been damaged and the degree of involvement of the central nervous system, one or more of the following may occur: spasms; tonal problems; involuntary movement; disturbance in gait and mobility; seizures; abnormal sensation and perception; impairment of sight, hearing or speech; and mental retardation. Early identification of cerebral palsy can lessen developmental problems and lead to appropriate intervention when it helps the most.
Associated Links
Cerebral Palsy Association of British Columbia
Epilepsy
Epilepsy is a neurological condition that from time to time produces brief disturbances in the normal electrical functions of the brain. Normal brain function is made possible by millions of tiny electrical charges passing between nerve cells in the brain and to all parts of the body. When someone has epilepsy, this normal pattern may be interrupted by intermittent bursts of electrical energy that are much more intense than usual. They affect a person’s consciousness, bodily movements or sensations for a short time.
Epilepsy may be treated with drugs, surgery, or a special diet. Of these treatments, drug therapy is by far the most common, and is usually the first to be tried. A number of medications are currently used in the treatment of epilepsy. These medications control different types of seizures. People who have more than one type of seizure may have to take more than one kind of drug, although doctors try to control seizures with one drug, if possible.
There are many students with epilepsy attending college. Most of them have a normal student life, fully participating in academic and social activities. Occasionally, individuals with epilepsy may appear to be sleepy or lethargic in class as a side effect from the anticonvulsant medication they take. After having a seizure, a student’s memory can be affected and accommodations may be necessary. Even with their medications, a few students will still experience seizures; however, not all seizures will be obvious to the teacher or classmates. Some mild seizures make the student appear to be briefly daydreaming, or the student may have a sudden involuntary body jerk.
There are a few students who sometimes have major seizures. These students are advised to alert their instructors of this possibility; however, due to the stigma associated with epilepsy, many refrain from telling anyone that they have epilepsy. If a student has a major seizure (commonly known as “grand mal”) while class is in session, the following suggestions should be helpful.
What should I do if a student has a seizure in class?
- Remain calm. Students will usually assume the same emotional reaction as the instructor. The seizure is painless to the individual.
- Notify Campus Health as soon as possible that a student is experiencing a seizure, (tell someone to make the call rather than leave the student).
- Move objects that might injure the individual having the seizure.
- DO NOT restrain the student or try to place objects in his or her mouth.
- Campus Health will determine if medical attention should be summoned for the individual.
- After a major seizure, the individual will have little or no memory of the seizure and will be physically exhausted. Following the seizure, the individual may need rest and sleep.
- Find out if a couch is available for use by an individual who needs to rest after having a seizure.
- A student who has epilepsy may encounter difficulty in concentration and in the ability to take accurate notes during lectures due to mild seizures.
Possible reasonable accommodations applicable for someone with epilepsy:
- Allow the use of a tape recorder for taping lectures and discussions.
- If the student cannot find someone to take notes, the faculty member could photocopy his/her notes for the student or announce (or have the student announce) to the class the need for a student volunteer to photocopy or make carbon copies of the lecture notes.
- Extended time for completion of tests.
Associated Links
British Epilepsy Association
American Epilepsy Society
Multiple Sclerosis
Multiple Sclerosis is an illness of the Central Nervous System in which two main parts differ: brain and spinal marrow. The fibres of the Central Nervous System are wrapped up and protected by a material called myelin (made up of proteins and fat) that facilitates the driving of the electric impulses among the nervous fibres.
In Multiple Sclerosis the myelin gets lost in multiple areas leaving scars (sclerosis); these injured areas are also known as of myelinoclasis plates.
The myelin protects and facilitates the operation of the nervous fibres, if the myelin is injured or it is destroyed, the ability of the nerves to drive electric impulses from and to the brain is interrupted and this produces symptoms appearance. In many occasions the lesion of the myelin is reversible.
Causes:
The cause of the Multiple Sclerosis is ignored, in spite of it, many scientists believe that the destruction of the myelin is the result of an abnormal answer of the immunologic system toward the own organism. That is to say, the immunologic system defends from the “intruders” like viruses and bacteria. In the autoimmune diseases, the organism attacks without warning the own tissue, in the case of Multiple Sclerosis, the attacked substance is the myelin.
Symptoms:
The symptomatology depends on the areas of the injured Central Nervous System and not all the people are affected in the same way, that is to say, the symptoms vary among different people and also in the same person according to the moment.
The symptoms include weakness, tingling sensation, fatigue, little coordination, balance problems, visual alterations, tremor, spasticity or muscular rigidity, dysfunctions of the speech, intestinal or urinal problems, unstable walk (ataxia), problems in the sexual function, heat sensibility , problems in the short term memory and occasionally reasoning problems (cognitive problems), although people that have Multiple Sclerosis have not got all these symptoms.
Diagnosis:
It cannot be diagnosed with a single test but rather some or all of the following procedures are required:
- A medical record in which the specialist will analyze signs and symptoms.
- An exhaustive neurological exam.
- “Evoked potentials” tests that measure the answer of the Central Nervous System in front of specific stimuli (noise, images, sensitive stimuli)
- The Magnetic Resonance, a relatively new form of visualizing precise and highly detailed images of the brain and spinal marrow.
- The lumbar puncture to analyze the composition of the liquid that wraps the spinal marrow (cephalorachidian liquid).
Women develop Multiple Sclerosis with more frequency (twice as much) than men. The diagnosis is usually made between their 20 and 40’s.
It is not hereditary, however studies reveal that certain family predisposition exists, then siblings or other near relatives have more probabilities of acquiring the disease.
Treatment:
Healing treatment of the Multiple Sclerosis is not known, but there are treatments to diminish the frequency or severity of the buds. For example, e muscular rigidity, sphincters alterations, depressive dysfunctions or mood, etc., are symptoms that can be satisfactorily treated in some patients.
For some people with this condition, the following strategies can be useful:
- Physiotherapy to help strengthen the weakened or uncoordinated muscles.
- Occupational Therapy is used to provide independence in daily life.
- Phonoaudiology helps those who have problems to speak or to swallow because of musculature weakness or little coordination.
Associated Links
Multiple Sclerosis of Canada
National Multiple Sclerosis Society
Muscular Dystrophy
The following information is excerpted from Muscular Dystrophy Association, Australia
The term “muscular dystrophy” covers over 40 separate neuromuscular disorders which have in common the progressive and irreversible wasting of muscle tissue. Some of these diseases are known as dystrophies, the wasting of the muscles from within themselves. Others are atrophies, wasting arising from a disorder originating in the nerve system which causes loss of the ability to use muscles. Various Myopathies, Peripheral Nerve and Metabolic Disorders also fall into the realm of disorders covered by the MDA’s program. These neuromuscular disorders (NMDs) are generally, incorrectly, termed “muscular dystrophy.”
Associated Links
Muscular Dystrophy Association of America
Credit:
MS Association Australia
Parkinson Disease
Parkinson is a gradual and progressive neurodegenerative disease that is characterized by presenting tremors at rest, abnormalities in walking and rigidity. It affects up to 1% of the 60 year-old grown-ups.
It is caused by a cellular degeneration of the cerebral base ganglia, those that are in charge of coordinating the posture movements and the fine motoricity. At the onset of the disease a functional alteration of these ganglia takes place due to a substance called dopamina deficit (neurotransmitter substance that allows the information nervous conduction).
Symptoms:
The first symptoms of the disease can be unnoticed, since they are unspecific and they mislead the diagnosis. They consist on great muscular fatigue, depression, widespread or located muscular pains. As time goes by rigidity appears, what hinders the extension and flexion of any corporal segment, the decrease of the movements (bradykinesis), the characteristic tremor(sign of the disease), the loss of the posture reflexes, deglutition difficulty, lacks of facial mimicry and lack of swinging movements during walking.
Treatment:
There is no cure for this disease, but drugs can be administered to improve the mobility. It should be kept in mind that when the disease begins clinically a very severe neuronal deterioration already exists inside the brain.
Besides the suitable treatment, physical exercise should be encouraged in the patient, useful in any stage of the disease, since the motor performance improves when walking, swimming or gymnastics.
A diet rich in liquids, proteins and fibres, is advisable since many patients present depressive syndromes, with possible constipation and malnutrition. Due to the immobility secondary osteoporosis can be presented.
Associated Links
Parkinson Information
Parkinson’s Disease Society of the United Kingdom
Tourette Syndrome
Tourette Syndrome (TS) is a neurological disorder characterized by tics —involuntary, rapid, sudden movements or vocalizations that occur repeatedly in the same way.
Diagnostic criteria include:
- Both multiple motor and one or more vocal tics present at some time, although not necessarily simultaneously.
- The occurrence of tics many times a day (usually in bouts) nearly every day or intermittently throughout the span of more than one year.
- Periodic changes in the number, frequency, type and location of the tics, and in the waxing and waning of their severity. Symptoms can sometimes disappear for weeks or months at a time.
- Onset before the age of 18.
Associated Links
Traumatic Head Injury
A traumatic brain injury (TBI) is an injury to the brain caused by the head being hit by something or shaken violently. This injury can change how the person acts, moves, and thinks. A traumatic brain injury can also change how a student learns and acts in school.
The term TBI is used for head injuries that can cause changes in one or more areas, such as: thinking and reasoning, understanding words, remembering things, paying attention, solving problems, thinking abstractly, talking, behaving, walking and other physical activities, seeing and/or hearing, and learning.
When an individual with TBI return to school, their educational and emotional needs are often very different than before the injury. Their disability has happened suddenly and traumatically. They can often remember how they were before the brain injury. This can bring on many emotional and social changes. The following tips may assist teachers in working with these students:
- Find out as much as you can about the persons injury and his or her present needs. Find out more about TBI.
- Give the student more time to finish schoolwork and tests.
- Give directions one step at a time. For tasks with many steps, it helps to give the student written directions.
- Show the student how to perform new tasks. Give examples to go with new ideas and concepts.
- Have consistent routines. This helps the student know what to expect. If the routine is going to change, let the student know ahead of time.
- Check to make sure that the student has actually learned the new skill. Give the student lots of opportunities to practice the new skill.
- Show the student how to use an assignment book and a daily schedule. This helps the student get organized.
- Realize that the student may get tired quickly. Let the student rest as needed.
- Reduce distractions.
- Be flexible about expectations. Be patient. Maximize the student’s chances for success.
ACQUIRED BRAIN INJURY
Causes of acquired brain injury can include, but are not limited to:
- Airway obstruction
- Near-drowning, throat swelling, choking, strangulation, crush injuries to the chest
- Electrical shock or lightening strike
- Trauma to the head and/or neck
- Traumatic brain injury with or without skull fracture, blood loss from open wounds, artery impingement from forceful impact, shock
- Vascular Disruption
- Heart attack, stroke, arteriovenous malformation (AVM), aneurysm, intracranial surgery
- Infectious disease, intracranial tumors, metabolic disorders
- Meningitis, certain venereal diseases, AIDS, insect-carried diseases, brain tumors, hypo/hyperglycemia, hepatic encephalopathy, uremic encephalopathy, seizure disorders
- Toxic exposure- poisonous chemicals and gases, such as carbon monoxide poisoning
Definition: Acquired Brain Injury
An acquired brain injury commonly results in a change in neuronal activity, which effects the physical integrity, the metabolic activity, or the functional ability of the cell. An acquired brain injury may result in mild, moderate, or severe impairments in one or more areas, including cognition, speech-language communication; memory; attention and concentration; reasoning; abstract thinking; physical functions; psychosocial behavior; and information processing.
Adopted by the Brain Injury Association Board of Directors, March 14, 1997.
Associated Links
Brain Injury Association of America
The Brain Injury Association of Canada
Vancouver Coastal Health
